Case 67
- Wangpan Shi
- Mar 9
- 2 min read
Here are three cases of bladder TURBT samples, please share your interpretations.
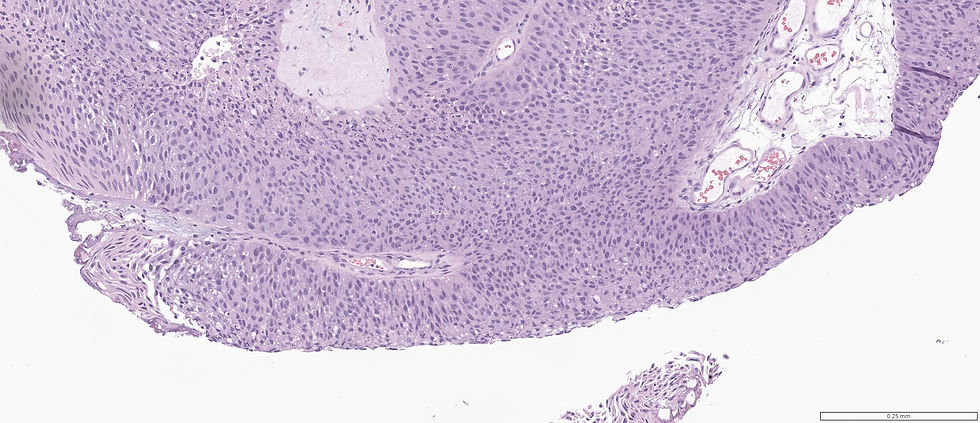
Case 1:



What's your diagnosis?
A. Carcinoma in situ
B. Dysplasia
C: Low grade papillary carcinoma, non-invasive
D: High grade papillary carcinoma, non-invasive
E: Invasive papillary carcinoma
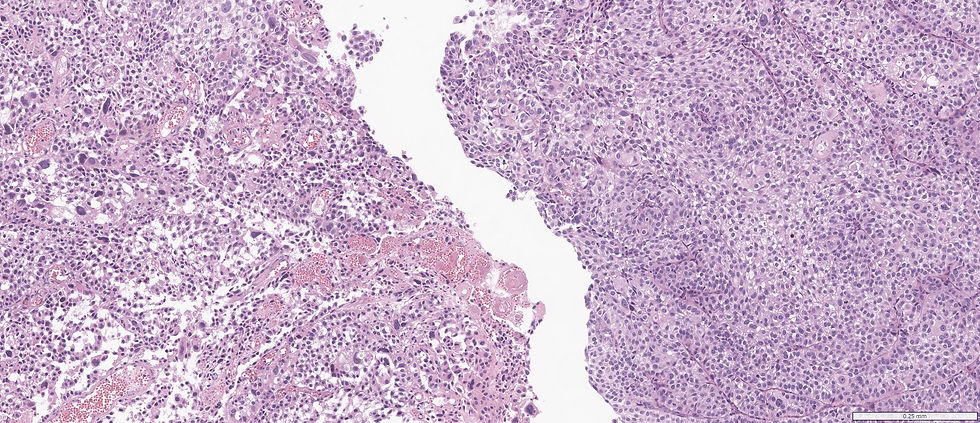
Case 2:


What's your diagnosis?
A. Carcinoma in situ
B. Dysplasia
C: Low grade papillary carcinoma, non-invasive
D: High grade papillary carcinoma, non-invasive
E: Invasive papillary carcinoma
Case 3:

3. What's your diagnosis?
A. Carcinoma in situ
B. Dysplasia
C: Low grade papillary carcinoma, non-invasive
D: High grade papillary carcinoma, non-invasive
E: Invasive papillary carcinoma
Answers for all three cases
Case 1: High grade papillary carcinoma, non-invasive; Case 2: High grade papillary carcinoma, non-invasive; Case 3: Invasive papillary carcinoma.
Feature | High-Grade Non-Invasive Papillary Urothelial Carcinoma (HGPUC) | Low-Grade Non-Invasive Papillary Urothelial Carcinoma (LGPUC) |
Architectural Complexity | More complex papillae with frequent fusion and branching. May show an inverted growth pattern. | Papillae are thinner and more orderly with fibrovascular cores. Some branching or fusion may be present but less pronounced. |
Cytological Atypia | Marked disorderly orientation of tumour cells with loss of polarity. Irregular, pleomorphic nuclei visible at low magnification. Nuclear hyperchromasia, prominent irregular nucleoli, and irregular nuclear contours are evident. | Mild nuclear atypia with mild loss of polarity. Scattered cells show nuclear hyperchromasia. Overall, nuclei display only mild variation. |
Mitotic Activity | Frequent mitotic figures, including atypical forms. | Occasional mitotic figures, generally located away from the basal layer. Lower mitotic activity than HGPUC. |
Nuclear Features | Significant nuclear size variation. Nuclear anaplasia may be present. | More uniform nuclear size. No marked variation in nuclear morphology. |
Growth Pattern | Can exhibit an inverted growth pattern, which may pose diagnostic challenges when differentiating from invasive carcinoma. Preservation of stromal–epithelial interface helps confirm non-invasiveness. | Inverted nests are usually thickened but maintain characteristics similar to LGPUC. The structures are more uniform compared to inverted papillomas. |
Risk of Progression | Higher risk of progression to invasive carcinoma. | Lower risk of progression compared to HGPUC. |
Case credit: UCSD Pathology
Author: Wangpan Jackson Shi, MD

Comments